Unraveling the ADHD Tapestry: ADD vs. ADHD
Have you ever heard someone use the term ADD and find yourself wondering: what actually is the difference between ADD and ADHD? What happened to the hyperactivity?
Don’t worry, it’s not anything new. It’s just an old, outdated term for the inattentive subtype.
In this article, we’ll discuss this, plus:
- The history and timeline of how and when attention deficit disorder (ADD) evolved to become ADHD.
- How we understand ADHD today compared to in the past.
- What we can expect in the future in terms of knowledge and understanding of ADHD.
Ready to jump into the ADHD journey and find out how ADD evolved into a more detailed, nuanced understanding of attention disorders? If so, keep reading.
The Evolution from ADD to ADHD
ADHD has come a long way in recent history as new research is constantly finding different ways to explain the complexities of ADHD and the way it affects the brain’s development and neurotransmitters. 🧠
We’re still far from a full understanding, but as you’re about to find out, a lot has changed in terms of how we understand and diagnose ADHD.
Let’s take a journey through the key dates that have defined how we describe ADHD today. 🗺️
1968: The DSM-II
Before 1968, the Diagnostic and Statistical Manual of Mental Disorders didn’t recognize ADHD (or any of its previous names), but that changed when the American Psychiatric Association (APA) released the second edition, the DSM-II.
This first introduced ‘Hyperkinetic Reaction of Childhood’. This early classification focused on hyperactivity but did not fully encapsulate attention deficits.
1980: The DSM-III
12 years later, the DSM-III was released with significantly revised psychiatric classifications. It introduced the new name ‘Attention Deficit Disorder (ADD) with and without hyperactivity’.
This was a pivotal moment, acknowledging that attention deficits could occur with or without hyperactivity, though scientists didn’t believe hyperactivity was a common symptom.
1987: The DSM-III-R
Over the next seven years, scientists found enough evidence to suggest that hyperactivity was actually a common symptom of ADD. To reflect this, the APA revised the DSM (DSM-III-R) to eliminate the distinction between ADD with and without hyperactivity.
They renamed it, Attention-Deficit Hyperactivity Disorder (ADHD). 🎉
This change aimed to emphasize the full range of symptoms beyond inattention, including hyperactivity and impulsivity.
1994: The DSM-IV
The DSM-IV introduced the three ADHD subtypes to better capture the disorder's diverse presentations.
These are:
- ADHD Predominantly Inattentive Type
- ADHD Predominantly Hyperactive-Impulsive Type
- ADHD Combined Type
This categorization further acknowledged the variability in how ADHD symptoms manifest.
2013: The DSM-5
At the time of writing this, the DSM-5 is the current and most recent version of the Diagnostic and Statistical Manual of Mental Disorders.
It continues to use the term ADHD but has further refined criteria to include examples relevant to adults, reflecting an understanding that ADHD is not just a childhood disorder but can persist into adulthood.
The DSM-5 also relaxed some criteria to make diagnosis more accessible to those whose symptoms significantly impair daily functioning.
As you can see, how we diagnose and understand the disorder's complexity and the diversity of its symptoms is continuously changing. This ongoing journey underscores the commitment within the medical and psychological communities to accurately identify and effectively support individuals with ADHD.
So why do people still use ADD?
ADD vs Predominantly Inattentive Type ADHD
Often when people still use the terms ADD and ADHD interchangeably, nearly 40 years after it was renamed, it’s either due to a lack of knowledge (that it’s outdated) or a way to deliberately highlight a lack of hyperactivity.
For those with purely inattentive symptoms, the common stereotypes (often harmful) that many people associate with ADHD, like being overly active, disruptive, or exhibiting reckless impulsive behaviors, don’t match their experience.
For a mental health professional to diagnose the predominantly inattentive presentation, they need to display six or more symptoms (for children) or five or more for an adult ADHD diagnosis.
These include:
- Often makes careless mistakes
- Has trouble paying attention and focusing
- Doesn’t seem to listen in conversation
- Difficulty following instructions
- Struggles with organization
- Avoids tasks that require sustained mental effort
- Forgetful and loses things frequently
- Gets easily distracted
As you can see, these symptoms are far less visible, and can, to some degree, escape the stigma that still surrounds hyperactive-impulsive symptoms. It’s unsurprising that some would use ADD as a way to try and avoid that stigma.
After all, many of us with ADHD are sensitive to rejection and will try to avoid it whenever we can.
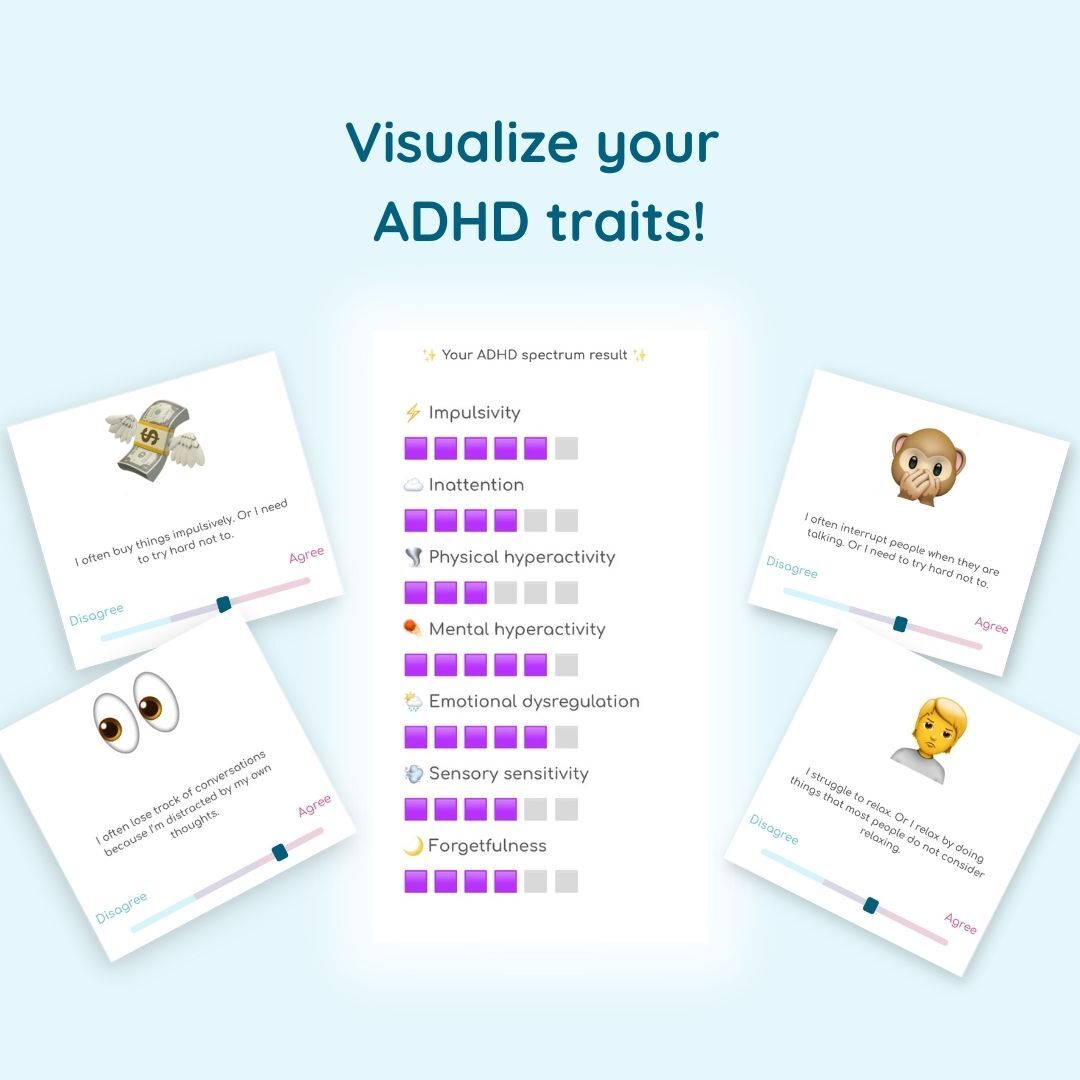
Take our fun online quiz to visualize your ADHD traits and learn more about your brain!
TAKE THE FREE TEST
Diagnosing ADHD Today: Where Are We Now?
We’ve talked a little about how the inattentive type of ADHD is diagnosed by healthcare professionals, but what about the diagnosis of Attention Deficit Hyperactivity Disorder as a whole?
Well, today, the process is more nuanced and holistic than ever before, emphasizing individual experiences and the impact of symptoms on daily life across different ages and settings. Let’s take a look at how.
1. Comprehensive Clinical Evaluations
These days, an ADHD diagnosis requires a thorough clinical evaluation, often conducted by a psychologist, psychiatrist, or pediatrician. This evaluation includes detailed interviews and questionnaires covering symptoms, childhood behavior (as an adult), school reports, and any previous diagnoses or treatments.
The goal is to gather a comprehensive picture of the individual's experiences and challenges in relation to their ADHD symptoms.
2. Recognition of ADHD in Adults
ADHD hasn’t always been recognized as a disorder that affects adults. In fact, until recently, you could only be diagnosed as a child, which explains why today so many adults are seeking diagnosis.
The adult diagnosis process considers life-long patterns of behavior, how symptoms manifest differently in adult responsibilities and relationships, and the presence of coexisting conditions, such as anxiety or depression.
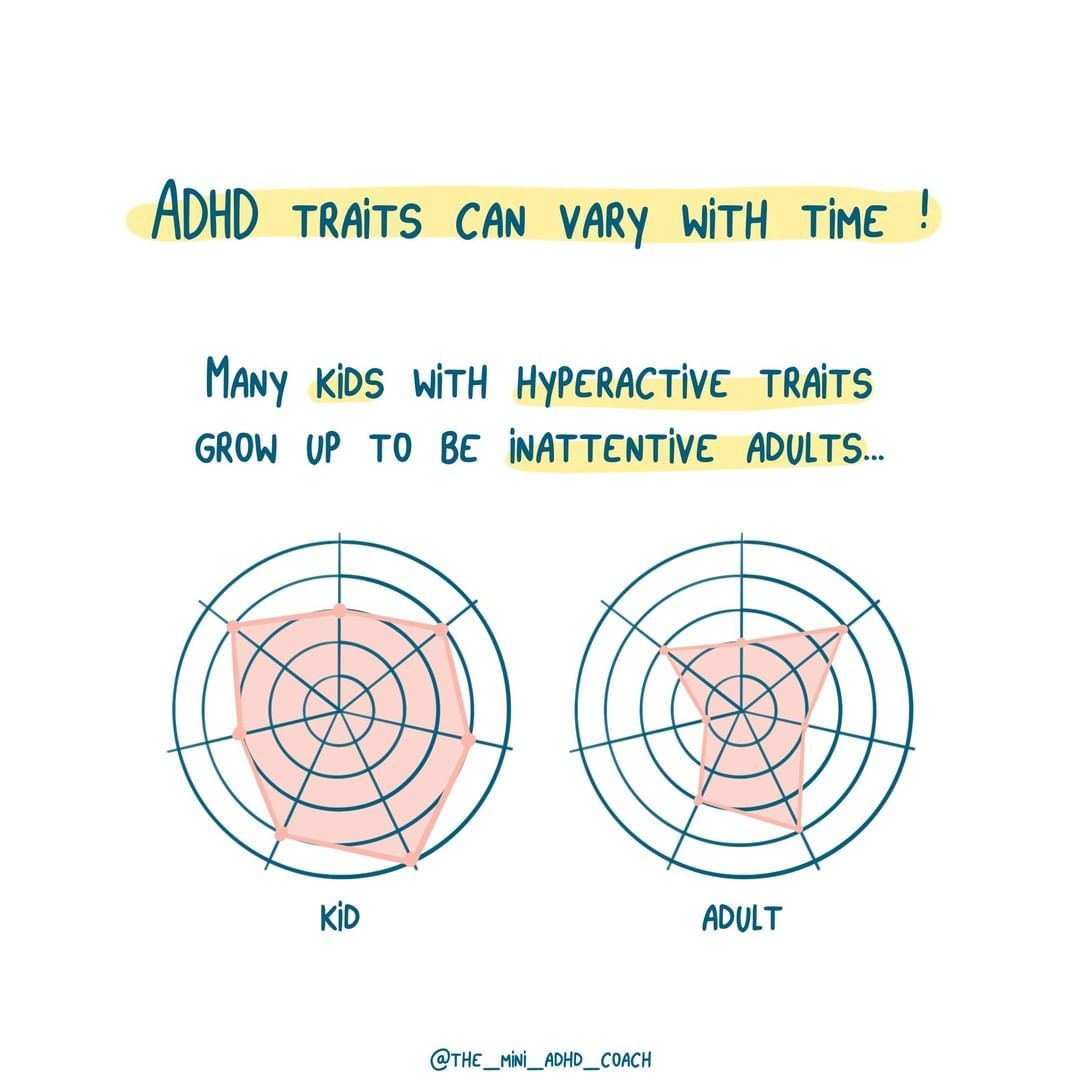
It’s also been acknowledged that ADHD traits and symptoms can change from childhood to adulthood, perhaps due to masking, learning to manage symptoms, or just changing as a person.
3. Criteria Adaptation
The current criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) now includes several updates, such as:
- Changing the age of onset symptoms to before 12 years (previously seven).
- Recognizing that symptoms can manifest differently depending on the individual's age.
- Allowing for ADHD diagnosis in the presence of other mental health conditions, including comorbidities.
4. Use of Rating Scales
Rating scales and checklists are now readily available to anyone who wants a way to help quantify the severity or frequency of their symptoms, and how they impact their daily lives.
These tools can be used by anyone, including parents, teachers, partners, or friends. Having people who know you offer their perspectives can help you understand how your symptoms manifest in different contexts like home, work, social situations, etc.
5. Emphasis on Impairment
A critical aspect of diagnosing ADHD today is the emphasis on impairment. It’s not just about having symptoms, but how these symptoms significantly impair academic, work, social, or personal functioning.
This shift ensures that diagnosis and subsequent treatment are tailored to improve quality of life and daily functioning, rather than diagnosis for diagnosis's sake.
6. Neuroimaging and Biomarkers
While not routinely used for diagnosis, there’s currently ongoing research into neuroimaging and potential biomarkers for ADHD. 🧬
The aim of these studies is to uncover the neurobiological underpinnings of ADHD, offering hope for future diagnostic tools and treatments.
It’s also pretty fascinating, isn’t it?
7. Awareness and Education
Arguably the most important change in recent years is the increasing awareness and education around ADHD as a society.
For too long, myths, misconceptions, and harmful stereotypes have stopped people from seeking the diagnosis and support they need and deserve. While we’re nowhere near full acceptance, there's now a growing understanding of the diversity of ADHD presentations, breaking down stereotypes and reducing stigma.
The Path Ahead
Diagnosing ADHD today involves a blend of scientific knowledge, clinical expertise, and a deep understanding of the individual's lived experience.
As we move forward, the focus continues to shift towards more personalized approaches that consider the full complexity of ADHD and its impact on individuals’ lives.
There’s still a lot of work to be done. Access to ADHD diagnosis and treatment is still limited in many countries, with multiple-year waiting lists and a shortage of professionals equipped to offer ADHD treatment like behavioral therapy and stimulant medication. This responsibility lies with the change-makers of our society.
But with all the ongoing research, evolving diagnostic criteria, and a growing emphasis on patient-centered care, the future holds promise for even more accurate and empowering ways to support those with ADHD. ☀️
Key Takeaways
- ADHD has evolved from 'Hyperkinetic Reaction of Childhood' (1968) to ADD (1980) and finally to ADHD (1987) to reflect advancements in understanding the complexity and diversity of symptoms associated with the disorder.
- Today, there’s a focus on comprehensive clinical evaluations for accurate diagnosis, considering symptoms, childhood history, and daily challenges.
- There’s now greater recognition of ADHD in adults, acknowledging lifelong patterns of behavior and how symptoms manifest in different life stages.
- Updated criteria in the DSM-5 now allow for a broader age range of symptom onset and consideration of comorbid mental health conditions.
- We all need to continue to increase awareness and education about ADHD to help break down myths, misconceptions, and stereotypes and encourage more individuals to seek diagnosis and support.
The evolution from ADD to ADHD is just one of the many ways our understanding of the neurodevelopmental disorder has changed over the years. As awareness grows and research progresses, it's as important as ever to advocate for improved access to diagnosis and treatment, ensuring individuals with ADHD receive the support they need to thrive.
Join us in raising awareness for ADHD in society so we can pave the way for a brighter and more inclusive future for everyone.
Visualize and assess 25 ADHD traits and understand how they affect your life.
Learn more-2.png)
Frequently Asked Questions (FAQs)
Is there a difference between ADD and ADHD?
The main difference is in terms. ADD (Attention Deficit Disorder) is an outdated term that has been replaced by ADHD, which includes both inattentive and hyperactive-impulsive symptoms.
How do I know if I'm ADD or ADHD?
If you struggle with focusing, are easily distracted, or act impulsively, you might have ADHD. A professional evaluation is needed to determine the specific type.
Why is ADD no longer a diagnosis?
ADD was replaced by ADHD in the 1990s to more accurately describe the range of symptoms, including hyperactivity and impulsivity, not just attention issues.